Policy. Analysis. Advocacy
Small-scale farmers
The importance of small farmersMicro, small and medium enterprises (MSMEs) play a critical role in the food system in developing countries. Worldwide, SME farms produce approximately 50% of calories, over 85% of fruits and vegetables and about 80% of meat and...
Mining: Bolivia’s environmental disaster
However, higher temperatures and fires are not what worries me the most. More severe damage to the environment, with long-term impacts, has been carried out for a long time now.
I am talking about the mining sector in Bolivia. This sector processes the minerals with very basic procedures and - in the case of gold – with great amounts of mercury, dumping mineral waste into rivers, contaminating the water, fish and all biodiversity in the river banks. Families downriver cannot eat the fish anymore and they even have high mercury levels in their bodies.
Digital tools for Monitoring & Evaluation
Data collection for development projects In rural areas far from internet service or in cities with electricity or internet access disrupted by violence or shortages, some #development projects still use paper and pen forms to collect information - primary stakeholder...
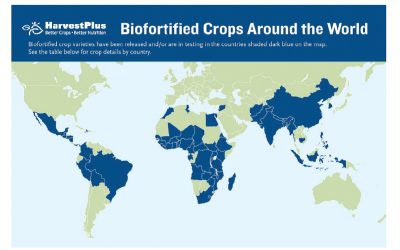
How to increase large-scale food fortification (LSFF)
Lack of micronutrients causes diseases ranging from anemia to stunting in children as well as child mortality and cognitive deficiencies. One key intervention is large-scale food fortification (#LSFF), which adds #micronutrients to food staples such as rice, wheat and...
The importance of food fortification
Approximately two billion people worldwide, at least one quarter of the world’s population, suffer from the “hidden hunger” of micronutrient deficiency. [1] Micronutrient deficiencyMicronutrients – vitamins and minerals such as Vitamin A, Vitamin B12, folic...
Ending Female Genital Mutilation (FGM)
Over 200 million women have undergone female genital mutilation (#FGM), a procedure where their vagina has been cut or mutilated. FGM occurs in over 90 countries in Africa, the Middle East and Asia, as well as in Europe, the US and other places people from those countries move. Learn tips on conducting outreach to communities where FGM occurs.
Universal Income
Instead of providing welfare payments to people who have to prove they have extremely low incomes, an alternative theory involves guaranteeing a basic income to everyone. The latest guaranteed income program is in Los Angeles county, California, USA. The Breathe program targets people with lower incomes who have been hurt by COVID-19. It will provide $1,000 a month to 1,000 people for 3 years, helping them “breathe easier”.
Helping Ukraine
(updated) How can you help the people in the Ukraine? By supporting #charities that support the people. At this point, it's most important to support humanitarian organizations, including those helping refugees. Liberico (lphr.org) https://lnkd.in/dQYpQfEm Vostok SOS...
The SDGs and businesses
22 November 2021 The UN's Sustainable Development Goals are targets for how we, on a planetary basis, need to restructure our economies, production, use of natural resources, and the living circumstances of men, women and children around the world. The 17 goals fall...
Non-communicable diseases (NCDs) and the poorest billion
NCDs and injuries among the world’s poorest 1 billion people; heart disease, asthma, diabetes, cancer, and mental health are a problem in developing countries.
How to promote public policy
Facts alone cannot win political debates. Facts do not conquer hearts. Too often scientists think the public will be swayed by facts. Read more on how to promote policies.
Public Health Priorities part 3: the US CDC
The budget for the US Centers for Disease Control and Prevention (US CDC) for FY20 was $7.9 billion, vs. the WHO’s 2019 budget of $2.2 B.
How should the funding pie be split?